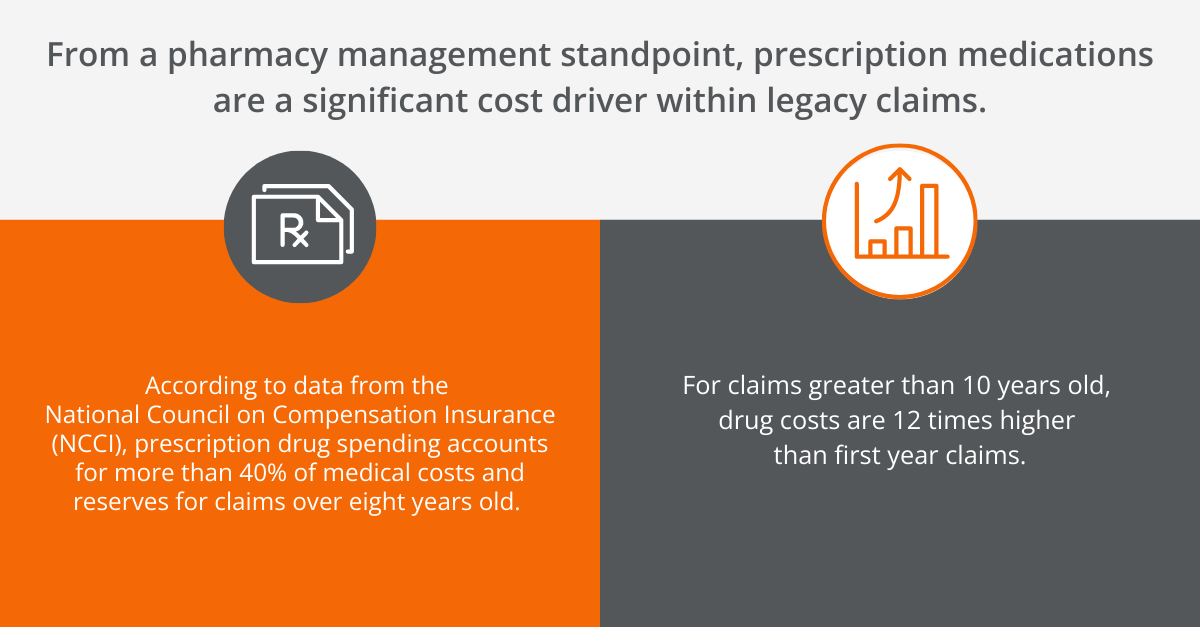
With workers’ compensation drug costs being an ongoing focus of attention, it’s essential for the pharmacy services sector to monitor one of the biggest cost drivers out there: legacy claims. Many pharmacy benefit managers (PBMs) in workers’ comp tend to downplay legacy claims because they are difficult to manage.
In fact, the vast majority of legacy claims we encounter at myMatrixx are inherited when a new client comes on board from a previous PBM. We have found that identifying and taking a proactive clinical management approach to these cases can result in millions of dollars in cost savings. For our existing clients, we use pharmacovigilance to “get ahead of the claim” and prevent these long-term, legacy claims from developing in the first place.
Most importantly, successful workers' comp case management for legacy claims can and should result in injured workers receiving a higher level of care and a better outcome.
What Are Legacy Claims?
Legacy claims, also called old claims or sometimes “old dog claims,” can refer to a number of situations. The exact time and circumstances it takes for a claim to reach legacy status can vary from carrier to carrier. Generally, workers’ compensation insurers will consider claims older than three-to-five years as legacy claims.
Often, legacy claims are cases that take longer than normal to reach the maximum medical improvement (MMI) needed for the injured patient to return to work. It can also refer to claims that have reached MMI, but still have ongoing care needs such as prescription medications or physical therapy. Additionally, legacy claims can be cases that involve some level of permanent disability.
In our decades of experience in helping clients effectively manage and resolve these difficult cases, myMatrixx has developed a proactive strategy for driving down costs and improving safety. Our focused expertise in case management advances our ability to prevent future legacy cases from developing.
Managing Inherited Legacy Claims
When finding ways to reduce drugs costs for long-term claims it is essential to understand the barriers that exist from an injured worker, prescriber and administrative standpoint, all of which drive costs year after year. In helping our clients resolve legacy claims that were not managed successfully prior to myMatrixx, our pharmacists regularly encounter several distinct phenomena.
For example, in a large number of cases, these injuries involve use of an opioid that the injured patient has potentially become dependent on. Prescription opioids should ideally be short-term aids that help injured patients dealing with injuries or recovering from surgery during the rehabilitation process. Not having a treatment plan with a clear endpoint and weaning plan in place can be a major contributor to pharmaceutical costs for legacy claims.
There are also hurdles that can prevent pharmacists and PBMs from intervening with prescribers, including ex parte laws that are present in many states. Administrative oversight is another contributor. Pharmacy costs in particular may seem “quieter” compared to other interventions such as surgery or physical therapy. Yet, not performing proactive reviews on these claims can become costly.
Just because they are difficult, doesn't mean legacy claims can't be managed. What these cases require is a higher level of intervention than newer claims. When managing inherited claims from other PBMs, myMatrixx leverages a comprehensive set of clinical pharmacy tools, including CARE Threshold Alerts, CASE Rx® reviews, and One Drug Reviews.
Getting Ahead of the Claim with Proactive Claims Management
For all clients we serve, preventing long-term cases is the other pillar of our approach to legacy claims. We call this our Get Ahead of the Claim StrategyTM – which means carefully planning comprehensive programs designed to keep pharmacy benefits on track from day one.
Our approach as a PBM is built on integrating analytics into clinical management supporting claims with targeted and actionable recommendations backed up by documented research. myMatrixx pharmacists, analysts, nurses and operations experts work closely with clients to provide individualized solutions for each case, including:
- Formularies customized for specific injured patients
- Support during discussions with treating physicians
- Recommendations on altering therapies
- Full case reviews when necessary
This type of proactive claims management enables myMatrixx to help clients reduce costs and improve outcomes for injured workers.
Making a Difference with Pharmacy Case Management
A great way to frame the interventions that pharmacists perform while managing legacy claims is through a concept we call “pharmacy case management.” Although pharmacists are not licensed adjusters, they can and do play a similar role in guiding these claims to ensure a positive outcome. In fact, an integrated partnership between clinical pharmacists and adjusters is an ideal strategy to drive down the cost of care and optimize outcomes. Furthermore, during the current talent shortage the industry is facing, our pharmacists provide an important safety net and enhanced efficiency if an inexperienced adjuster is involved with a legacy claim.
myMatrixx Legacy Claims Client Case Study
Get an in-depth look at our Legacy Claims Management program.
By working closely in these cases to ensure injured workers are receiving correct pharmaceutical care, clinical pharmacists are critical to keeping these cases on track. As just one example, a pharmacist can explain the benefits of a weaning program if a new prescribing physician is identified ordering opioid medication after an injured worker reports pain during the recovery process. Intervening at key junctures can represent a major turning point between a short-term claim and a legacy claim.
In one of our most successful cases of legacy claims management, myMatrixx was able to help a new third party administrator (TPA) client resolve a 10-plus-year case that had involved multiple surgeries and medication dependence. Through collaboration between myMatrixx pharmacy case management, the TPA client, the rehab facility and family members, the case was successfully closed and the injured worker was able to return to work.
Need help managing legacy claims in your portfolio? Contact our Sales team for more information and get started today.