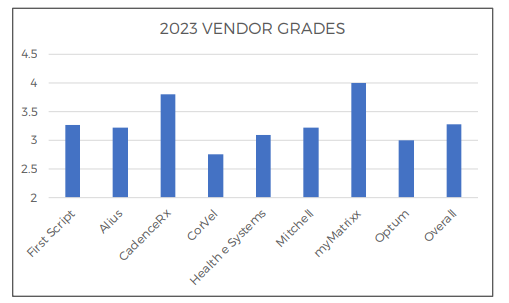
The industry has spoken and MyMatrixx by Evernorth continues its streak of being ranked the #1 pharmacy benefit manager (PBM). CompPharma, an independent consulting and research firm, surveyed 31 workers’ compensation professionals including decision makers, clinical personnel, and operations staff in state funds, carriers, self-insured employers, guarantee funds, and third-party administrators on the top PBMS and topics such as drug spend, pharmacy programs, and industry trends.
Combining their input with analysis of pharmacy data from 2022 and 2023, CompPharma released their 19th Annual Prescription Drug Management in Workers’ Compensation survey report.MyMatrixx earned the #1 ranking by the industry, a position we have held since 2019.
The overall score for all PBMs was 3.28. MyMatrixx retains the crown among all respondents for the fourth straight year with an average grade of 4, which is about 15% higher than the average score. Scores were based on perception of each PBM, including both reputation and firsthand experience, with “1” being “would not work with” and “5” being “would highly recommend.”
Helping MyMatrixx reach the top spot was our excellent customer service. Customer Service is ranked as the most important PBM attribute and was highly correlated to vendor grades.
Top Drug Spend Takeaways
- There was a 4% increase in drug spend overall and a 3% average increase per respondent.
- Opioid spending decreased by 8.7% overall and at an average of 7.85% per respondent. This is significantly lower than prior years where the decrease was in the double digits.
- Just 9.1% of overall drug spend was on opioids; down from a figure that was stuck in the low teens for several years.
What the Industry is Talking About
- Physician dispensing continues to be a polarizing issue with 42% of respondents rating it as little impact on the industry and another 42% rating it as high impact on the industry.
- Eighty-four percent of respondents are generally supportive of alternative pain management options including technology ideas and several behavioral health programs.
CompPharma, an independent consulting and research firm, works with payers and pharmacy benefit managers (PBMs) to bring transparency into workers’ compensation pharmacy programs. Since 2004, the firm has surveyed workers’ compensation payers on managing the cost of prescription drugs. The goal of the survey is to gain insight into the major cost drivers, management approaches, problems and trends that decision makers face — and how they are working to control costs and meet clinical goals.
We’re proud to set the standard in delivering the best client and customer service in the industry, earning us the title of top PBM by independent industry research group CompPharma.